Revenue Cycle Management 101: From Patient Check-in to Payment
By Billmate
Oct. 1, 2025, 5:50 a.m.
Introduction
In today’s healthcare system, revenue cycle management (RCM) is the backbone of financial stability for hospitals, clinics, and physician practices. From the moment a patient checks in until the final payment is collected, RCM ensures accurate billing, faster reimbursements, and reduced claim denials. Despite its importance, many providers continue to struggle with inefficient processes, rising administrative costs, and compliance challenges. This guide explores the complete medical billing revenue cycle, key challenges, and proven strategies to optimise healthcare billing in 2025.
What is Revenue Cycle Management?

Revenue cycle management is the financial process that tracks patient care episodes from registration to the final payment. In healthcare, RCM integrates medical billing, coding, insurance verification, and patient collections into one streamlined process. By focusing on both clinical and administrative functions, RCM ensures providers can deliver quality care while maintaining financial health.
Why Revenue Cycle Management Matters for Healthcare Providers
-
-
Reduces claim denials and rejections through accurate data entry and coding
-
Improves cash flow by accelerating reimbursements
-
Ensures compliance with HIPAA and CMS guidelines
-
Enhances patient satisfaction with transparent billing and payment options
-
For clinics and hospitals, strong healthcare revenue cycle management is not optional—it’s essential for sustainability.
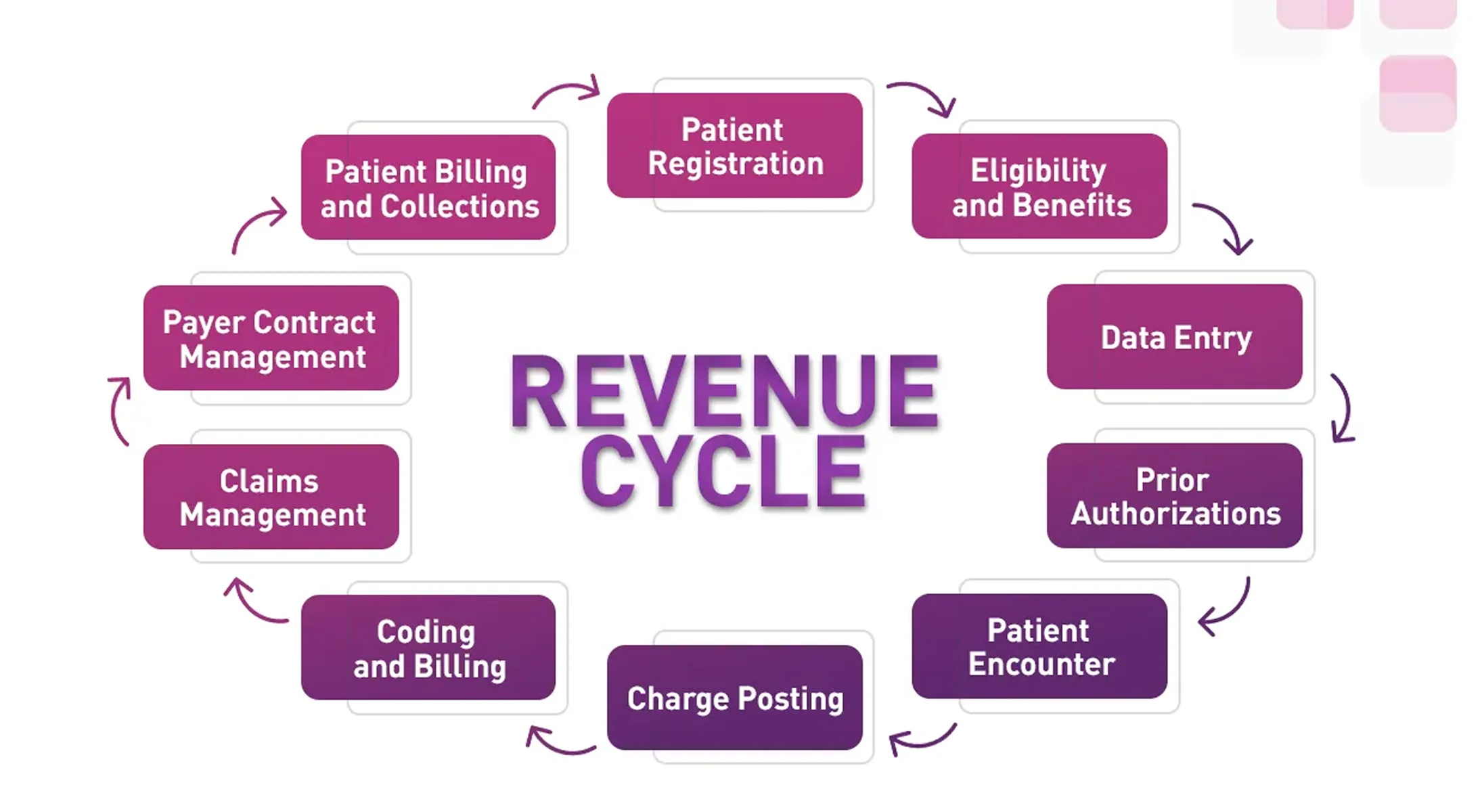
Steps of the RCM Process: From Patient Check-in to Payment
-
Patient Registration and Eligibility Verification
Accurate demographic entry and insurance eligibility checks reduce future rejections.
-
-
Real-time insurance verification helps prevent common causes of claim denials.
-
Collecting co-pays upfront improves the patient payment collection strategy in RCM.
-
-
Charge Capture and Medical Coding
Providers document services, while coders translate them into standardised CPT, ICD-10, and HCPCS codes. Errors in this area often result in medical billing claim denials.
-
Claim Submission
Clean claims are submitted electronically to payers. Utilising automated systems enhances accuracy and minimises delays.
-
Payment Posting and Processing
Insurers process claims and post payments. Any discrepancies require immediate follow-up to avoid accounts receivable in healthcare backlogs.
-
Denial Management and Appeals
If a claim is denied, the denial management process begins. Effective appeal strategies recover revenue and highlight workflow weaknesses.
-
Patient Billing and Collections
Patients receive bills for their share of the responsibility (deductibles, co-insurance). Clinics with clear communication and flexible payment plans tend to have higher collection rates.
Common Challenges in Revenue Cycle Management for Small Clinics

-
-
Limited staff training on billing and coding
-
Lack of automated claim scrubbing tools
-
High administrative burden with manual processes
-
Patient dissatisfaction due to unclear billing
-
Rising compliance demands (HIPAA, CMS updates)
-
These challenges often result in delayed payments, claim denials, and cash flow problems.
Best Practices to Optimise Revenue Cycle Management
-
-
Implement automation: AI-driven billing software reduces medical billing errors.
-
Regular staff training: Keeps coders updated on changes in ICD-10 and payer rules.
-
Proactive denial management: Track denial trends and fix recurring issues.
-
Outsource RCM services: Many small providers choose to outsource revenue cycle management to reduce costs and gain expert support.
-
Patient engagement: Offer digital portals, e-billing, and flexible payment plans to improve collection rates.
-
Geo-Focused RCM Insights
In the USA, RCM services are increasingly outsourced to manage growing compliance complexity. In countries like Pakistan, medical billing RCM in Lahore and Karachi is gaining attention as providers modernise their systems. This makes outsourced revenue cycle management a cost-effective solution for small healthcare providers, both locally and internationally.
Future of RCM in 2025 and Beyond

The future of medical billing revenue cycle management lies in:
-
-
AI-driven claim scrubbing and coding assistance
-
Blockchain-based billing security
-
Advanced EHR/EMR integration with billing systems
-
Predictive analytics to forecast denials and revenue patterns
-
These innovations will redefine healthcare billing, making it faster, more accurate, and patient-centred.
Conclusion
Revenue cycle management is the lifeline of healthcare organisations. From patient check-in to payment collection, each step must be managed with precision to ensure financial stability and patient trust. By adopting automation, outsourcing RCM services, and adhering to best practices, clinics and hospitals can reduce claim denials, enhance revenue flow, and deliver improved patient experiences.
Ready to streamline your billing and maximise reimbursements?
Schedule Your Free Consultation Today with BillMate and discover how our RCM expertise can transform your practice.
Frequently Asked Questions
1. How does revenue cycle management work in clinics?
Revenue cycle management (RCM) in clinics begins at patient check-in, where insurance eligibility and demographic details are verified. It continues through charge capture, claim submission, denial management, and ends with patient payment collections. Clinics that adopt automated billing software can streamline this process, reduce errors, and maintain a healthier cash flow.
2. What does RCM from patient check-in to payment include?
The RCM process from patient check-in to payment includes multiple steps: verifying insurance coverage, coding medical services, submitting claims, tracking denials, and collecting patient balances. Each step requires accuracy, as even minor medical billing errors can result in rejected or delayed payments.
3. What are the common challenges in revenue cycle management for small clinics?
Small clinics often face challenges such as high claim denials, staffing shortages, outdated billing systems, and difficulty collecting patient balances. These issues can slow down cash flow. Outsourced revenue cycle management services help small clinics overcome these barriers by offering experienced billing professionals and modern technology.
4. What are the steps of medical billing and revenue cycle management?
The steps of medical billing and RCM include:
- Pre-authorisation & eligibility verification
- Charge capture & medical coding
- Claim submission to payers
- Denial management & appeals
- Accounts receivable follow-up
- Patient payment collection
By following these steps precisely, healthcare providers can improve claim acceptance rates and minimise denials.
5. How can outpatient clinics optimise revenue cycle management?
Outpatient clinics can optimise RCM by using electronic health records (EHR) with integrated billing systems, training staff on claim submission accuracy, and implementing denial management strategies. Automation tools also reduce repetitive tasks and speed up reimbursements.
6. What are the RCM best practices for physician practices?
Best practices include accurate documentation, proactive eligibility checks, coding compliance, and timely claim submissions. Physician practices that use RCM best practices often experience reduced claim denials and faster payment cycles.
7. How can effective revenue cycle management reduce claim denials?
Effective RCM reduces claim denials by addressing errors before claims are submitted. This includes eligibility verification, coding audits, and implementing a denial management process. Studies show that up to 90% of claim denials are preventable with proactive RCM strategies.
8. Is outsourced revenue cycle management beneficial for small healthcare providers?
Yes. Outsourced RCM services provide small healthcare providers with access to billing experts, advanced software, and compliance monitoring, all without the need to hire full-time staff. This helps improve cash flow, reduce administrative burden, and increase claim acceptance rates.
9. What is the best patient payment collection strategy in RCM?
The best strategy includes clear communication of financial responsibility at check-in, offering multiple payment options, and using automated reminders. Practices that follow a structured patient payment collection strategy often recover a higher percentage of balances on time.
What To Read Next

By Billmate | February 23, 2026
Hospice Modifiers GV and GW: A Complete Guide for Medicare Billing
In-depth 2026 guide to hospice modifiers GV and GW, Medicare billing rules, documentation standards…

By Billmate | February 20, 2026
Tick Bite ICD-10 Codes and Billing Guide for Accurate Medical Coding
Complete guide to tick bite ICD-10 codes, Lyme disease coding, CPT tick removal billing, erythema m…

By Billmate | February 19, 2026
Denial Management in Medical Billing: Common Denials, Causes, and Prevention Strategies
Learn denial management in medical billing, common denials, eligibility denials, causes, prevention…

By Billmate | February 17, 2026
Mastering Revenue Cycle Management in Healthcare: A Comprehensive 2026 Guide
A comprehensive 2026 guide to revenue cycle management in healthcare, RCM in medical billing, hospi…

By Billmate | February 12, 2026
Patient Responsibility in Healthcare: How Providers Can Improve Collections Without Hurting Patient…
Learn how providers can improve patient responsibility collections without damaging trust, transpar…
Join our team to be a part
of our story
Learn more about our career, education and
posting jobs, and
submit simple application.